Metal on metal hip resurfacing can now be accomplished with fully porous bone ingrowth femoral and acetabular components. In March of 2007, after 8 years of working to perfect the surgical techniques and implants for resurfacing, I believe that I finally was able to perform a hip resurfacing that may last a lifetime in most young patients. In March 2007 I implanted the first BIOMET POROUS RECAP and MAGNUM combination hip resurfacing.


Cemented femoral component

You might ask; what is so special about this?
Let me explain. I believe cement fixation is the weakest link in an otherwise very durable hip reconstruction. I have finally been able to eliminate the cement!
When hip resurfacing first re-emerged as an option with metal-metal bearings in the early 1990’s in England and Austria, it was already clear to many hip surgeons that the method of fixation of the implant to bone with cement, and the plastic bearing were the two weakest links of a total hip arthroplasty.
By that time, porous ingrowth fixation had already been determined to be superior to cement in socket components in stemmed total hips; most surgeons were already using them routinely. In fact, I was an orthopedic resident at Johns Hopkins at that time; I never even implanted a cemented socket during my training. Porous ingrowth fixation was already emerging as superior to cement for the stems of total hips at that time, but I still did cement a few during training. Cement fixation of hip implants was clearly being surpassed by porous ingrowth fixation at that time. This trend has only continued over the last 15 years
But we did not have a solution to replace the plastic bearing in the early 1990’s. Although thick plastic sockets were durable enough as a bearing surface for small bearing stemmed total hips in old inactive patients, they did not work well when they were implanted in young active patients, or when the plastic bearings were required to be large and thin as for hip resurfacing.
By 1990, the Sulzer Orthopedic Company in Austria had made a breakthrough! They figured out how to build proper metal–metal bearings for total hips, and found they were 100 xs more wear resistant than plastic. Both Heinz Wagner and Derek McMinn immediately got the idea to apply metalmetal bearings to the previously abandoned concept of hip resurfacing. Finally the thin bearing surfaces required for hip resurfacing could be made out of cobalt-chrome (CC), an extremely durable and wear resistant metal.
In Dr. Wagner’s resurfacing prosthesis, which had a metal-metal CC bearing, bone attachment was achieved by a roughened titanium surface (on the backside) pressed into bone without cement and without a true porous ingrowth surface. It is not surprising that these had a high failure rate; they did not remain fixed to the bone long.
Mr. Derek McMinn (“Mr.” is usually the preferred title for senior surgeons in England), on the other hand, tested several bone attachment methods in his earliest attempts at hip resurfacing**.Not surprisingly, he found that porous ingrowth surfaces were superior to cement fixation and to roughened metal pressed into bone on the socket side. As I mentioned previously, we were already exclusively using porous ingrowth sockets in all total hips at that time. On the femoral side he tested cement, roughened surfaces, and roughened surfaces with sprayed-on bone mineral (hydroxylapatite or HA). He did not test porous ingrowth fixation on the femoral side. He was working with Corin at that time, and I believe they were unable to manufacture an adequate porous femoral component at that time. Initially he discovered that the cemented and HA femoral components were equivalent for the first 2 years of service, but that both were superior to plain roughened metal surfaces. I am not certain why he chose cement over HA for his preferred femoral fixation at that time. Nevertheless, when he started Midlands Medical Technology and produced the Birmingham Hip, He had decided on a porous plus HA socket fixation and cement fixation for the femur. We call this type of fixation “hybrid” because one component uses cement and the other uses bone ingrowth.
The rest is history! Derek McMinn was able to revive the hip resurfacing concept with a metal-metal bearing and a reliable form of fixation to bone. He and numerous others can now show 95% survivorship in hip reconstructions in young patients at 7 years, and even 99% survivorship in ideal candidates at 8-10 years. Previously metal plastic total hips could only achieve 70-80 % survivorship in young patients at 7 years. Two additional major advantages he made possible for young people were to preserve their bone stock for future surgery, if this was required, and to virtually eliminate hip instability. Hip dislocations that occurred in 5% of 28mm metal-plastic total hip bearings, almost never occur with hip resurfacing.
When I first began performing Hip Resurfacing in 1999, Derek McMinn’s early 2 year data were available. I was drawn to the procedure because it was a bone sparing alternative for the younger more active patient. It appeared that metal-metal bearings might solve the primary problem that caused the previous metal-plastic resurfacings to fail. I felt it was worth exploring.
The only thing that puzzled me was why cement was chosen as the fixation method on the femur? It was already abundantly clear that porous ingrowth fixation was superior for socket and stemmed components of total hips, particularly in the younger more active patients. Why then would you use cement to fix a femoral component in hip resurfacing, an implant specifically intended for the young highly active patient?
I began working with Corin (Mr. McMinn’s first corporate partner in resurfacing). In 1999 they were unable to build a porous femoral component at my request. I convinced them to modify Mr. McMinn’s earliest HA component by adding three longitudinal placed derotation splines on the bone side. I have just published a 7 year report on this implant (1). 15/15 femoral components are still well fixed. This is only a small group, but it does show that the femur may be able to achieve fixation long term without cement.
In 2001 I decided to take a different approach. I worked with Corin to plan, implement and successfully complete the first US FDA Study of metal-metal hip resurfacing devices. As the principal investigator and initial study site of this 12 center FDA trial, I performed nearly half of all the procedures that eventually led to FDA approval of the Cormet 2000 resurfacing device in January 2007. This device has porous (plus HA) socket fixation, and cemented femoral fixation (hybrid fixation).
Because Corin was unable to build an uncemented femoral component to my specifications, I looked for other manufacturers who might be able to do it. There were two challenges. First, an even porous coating had to be applied on the inner surface of the femoral component. This is technically much more difficult than applying a coating to the outside of a socket component. Second, a very precise set of bone measuring and cutting tools had to be developed to reliably and reproducibly prepare femoral heads so that the femoral component could be tightly wedged on. When we were done preparing the femur, ideally the femoral prosthesis would fit so tightly that you should not be able to manually budge it on bone of various different densities. Also there should be no gaps between the bone and the porous surface. Instruments available for cemented components at that time did not require nearly this precision, because by its very nature, cement acts as a grout to fill all the gaps between the implant and the bone.
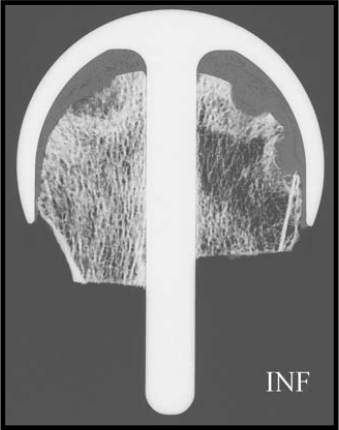
Section of a well functioning cemented femoral component.
Note: thick cement layer that has penetrated into bone
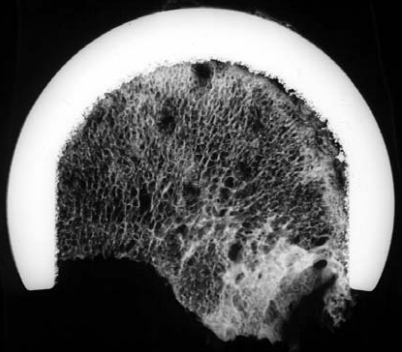
Section of an uncemented femoral component.
Note: close application of bone to the porous coating on the femoral undersurface
There was one company that was willing to take on this challenge. BIOMET is the worlds 5th largest manufacturer of orthopedic implants. They had already developed metal-metal bearings at this time, but had not ventured into the field of resurfacing. In December 2004 I implanted the first BIOMET Recap/Magnum resurfacing in the US. It had porous fixation on the socket and cement fixation on the femur (hybrid fixation). The more accurate instrumentation required for porous femoral implants were now available, but we still had more work to do on perfecting the porous femoral component itself. Finally, in March 2007, 6 years after starting the BIOMET project, I was able to implant the world’s first fully porous metal-metal hip resurfacing.
Meanwhile Corin also developed an improved uncemented femoral component. Their device was released in 2004 in England. It is only partially porous coated, but does have HA coating on the entire undersurface. They did beat me to the market with my idea, but they were not able to deliver a fully porous coated device. It is not available in the US.
I have now implanted over 300 of the fully porous BIOMET devices. In every case I have achieved a very tight initial press fit to the bone. In no case have I had to abandon my operative plan for technical reasons. So far I have had three femoral neck fractures. This 1% rate is unfortunately no different than the rate of femoral neck fracture that I have been able to achieve in 1200 cemented femoral components that I have done previously. I have had the following complications:
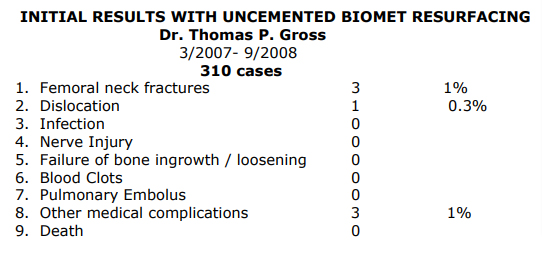
There have been only 3 revisions; these were the cases where femoral neck fractures occurred. One was in a woman with normal bone density and two were in men with osteopenic (mildly weak) bone. The postoperative regimen for uncemented resurfacing is identical to the one I use for my hybrid resurfacing. I have been able to detect no difference in the speed of recovery and early satisfaction between the previous hybrid fixation group and the new uncemented group.
I must caution you that these results are very preliminary. Although I am very enthusiastic about this implant system, I believe it will take at least two years of XR follow-up before I can be certain that the femoral component has achieved bone ingrowth in any one particular patient. When I have at least 100 patients with 2 year XR, I will submit my data for publication.
At this point the BIOMET porous Recap femoral component is FDA approved for femoral resurfacing. There is no other porous femoral component available in the US that is suitable for metal-metal resurfacing. Corin has developed a partially porous femoral component elsewhere in the world. At this point (except for one single component) I am the only surgeon to implant the Biomet porous Recap device. Biomet has now been able to step up their production so that I have enough devices to implant any patient who chooses to have uncemented resurfacing. BIOMET is poised to release this implant to other surgeons who wish to begin using it soon. I suspect that most other manufacturers of resurfacing devices are working on developing similar uncemented femoral components. I predict that in 1-2 years most companies will be offering this option. Other surgeons who are currently critical of uncemented resurfacing will soon move to this method when their company starts producing such a device.
At this point I am aware of 4 other surgeons in England who have experience with bone ingrowth type uncemented femoral components. They have all used one (of the two versions) of the Corin uncemented femoral components that I have described above. If we combine the results of Mr. Damien Griffen, Mr. Richard Villar, Dr. Spriggins, Mr. Darren Fern we have a total of over 600 patients with 1-3 year follow-up. These patients with uncemented resurfacing have similar early results as we have seen for cemented femoral components. Mr. Villar’s study was actually a direct comparison of a hybrid Birmingham to an uncemented Corin device; he found no significant difference at 2 years.
There is one other question that still needs to be addressed. Why has cement held up so well in young active resurfacing patients? After all, we can achieve 95% durability for 7 years after surgery and even 99% at 9 years in selected patients. When I first started performing resurfacing surgery, only 2 year results were available. I am now actually surprised how well cement has held up as a method for femoral component fixation at 7 years in these patients. The best explanation that I can find for this phenomenon is that cement is loaded in a very favorable fashion under a cemented femoral resurfacing component. On the socket side of all hip implants, and around the stem in total hips, cement is often repetitively loaded with shear forces. Cement is known to perform poorly under these types of loading conditions in the laboratory. Under the resurfacing femoral component, cement is exposed to primarily compressive forces. Cement is strongest under these conditions. (But bone ingrown porous surfaces are superior to cement interfaces in all loading conditions). Although cement holds up reasonably well in femoral resurfacing, I believe that it is still the weakest link in the hip resurfacing construct and that it will be the primary cause of late failures after 10 years.
Earlier, I explained that by the early 1990’s it was already clear that bone ingrowth type uncemented fixation was definitely superior to cement for total hip sockets and probably for femoral components as well, particularly in the young patient. Today, in the US, 95% of all sockets and 80% of all stems implanted in total hips are porous ingrowth types. Porous ingrowth is a more reliable and durable method of fixation in the hip.
Why are we then still using cement to attach femoral resurfacing implants to bone in the hips of young active patients?
Some experts answer this question by stating that cement acts as a material of intermediate stiffness to better transfer stress from the rigid implant (Cobalt-Chrome) to the much more flexible bone. This sounds interesting, and perhaps even somewhat scientific. But why then does the socket component in the same resurfacing patient fare better if it is attached to bone directly with a porous surface instead of with this “ideal stress transferring” cement? Why do total hip stems perform better in young active patients if they are attached to bone directly by porous ingrowth rather than by cement?
Why are we then still using cement to attach femoral resurfacing implants to bone in the hips of young active patients?
Some experts answer this question by stating that they are not certain that the blood supply of the femoral head after resurfacing surgery has an adequate blood supply to allow bone ingrowth into a porous coating. This is a valid concern. There are many facts to consider. There is no question that the blood supply of the femoral head is temporarily impaired after resurfacing. Approximately 1% of patients suffer a femoral neck fracture within 6 months of surgery (partially) because of this problem. In these cases the pathologist can determine that the femoral head was avascular (dead) after the surgery and prior to the fracture. In some patients the femoral head crumbles more slowly and presents as a loose implant within 12 years after surgery. If femoral heads that have been resurfaced are harvested before 1 year postop for reasons other than femoral failure (a rare event), an area of avascular bone is seen in the top of the femoral head with an adjacent healing response. Beyond 1 year the heads are seen to be completely viable if harvested.
The evidence is far from conclusive, but I believe that in virtually all resurfacing patients a portion of the top of the femoral head is avascular immediately after surgery. The size of the dead zone varies. If most of the head is avascular and the bone is weak and if the patient increases his activity too quickly after surgery, the femoral neck may fracture. Some combination of these factors results in fracture in 1 % of patients. However, in most patients, the bone recovers and the resurfacing works. If a fully porous coated implant is wedged tightly onto the head, will it achieve ingrowth? The vast majority of femoral heads are only avascular in the apex (very top of the head). In a fully porous device the coating is in direct contact with viable bone at the base of the head and the device is firmly wedged onto the bone allowing no micro motion. These are the prerequisites for bone ingrowth. Tight initial press-fit fixation and a porous ingrowth layer of metal sitting adjacent to viable bone. Even a device that is partially porous like the Corin uncemented still has HA adjacent to the viable bone at the base of the head. Initial attachment could occur to this HA. When the head fully heals, the bone may also grow into the porous portion of the implant in the apex giving a more durable long term fixation. Theoretically this appears to be a slightly less favorable situation, but it is likely to work in my opinion.
Congratulations that you have made it through my very brief discussion of this very complex topic! The jury is still out. Cleary my preference is an uncemented femoral component and most of my patients follow my recommendation. However, I still cement some femoral heads at the request of patients who are not comfortable with the porous femoral option.
In summary:
♦ Fully porous femoral resurfacing components are now available in the US from Biomet.
♦ These components allow us to eliminate cement completely from the resurfacing procedure.
♦ No other companies are yet selling these in the US.
♦ Corin has had a partially porous femoral component available in Europe for several years.
♦ Virtually all clinical data on hip surface replacement to date is based on an uncemented acetabular component and a cemented femoral component (hybrid fixation).
♦ Corin data from England with a partially porous femoral components is equivalent to data with cemented femoral components at 1-3 years in over 600 patients.
♦ My limited 7 year data with a Corin HA nonporous uncemented femoral component is promising.
♦ It is not clear, if uncemented technology on the femur will be better or worse then cemented femoral components at this point.
♦ I perform either the traditional hybrid or the latest fully porous resurfacing as desired by the patient. My preference is the uncemented technique.
♦ If uncemented hip resurfacing proves to be equal to hybrid fixation at 2 years, then most surgeons will agree with me that the long term outlook almost certainly will be better for the uncemented method. The entire resurfacing market will then switch rapidly to uncemented fixation.
References:
1. Gross, T., Liu, F. Metal-on-Metal Hip Resurfacing with an Uncemented Femoral Component. Journal of Bone and Joint Surgery American 2008; 90 Supplement 3: 32-37.
2. McMinn, D., Treacy, R., Lin, K., & Pynsnnt, P. Metal on Metal Surface Replacement of the Hip: Experience of the McMinn Prosthesis. Clinical Orthopaedics and Related Research, 1996 (329S):S89-S98.




