HIP RESURFACING:
CONTROVERSIAL TOPICS:
- Which bearing type is more prone to wear related failure?
- Which procedure is least invasive?
- Which procedure has a faster recovery?
- Which procedure has more long-term data?
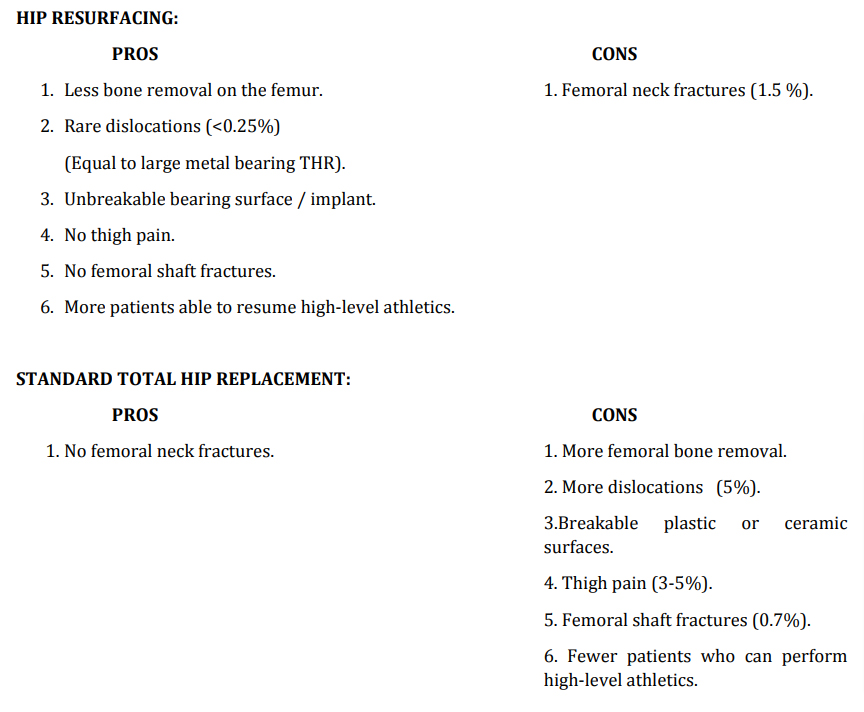
- Considerably less bone is removed on the femur in hip resurfacing (HR) than in standard stemmed total hip replacement (THR). This makes revision surgery on the femoral side less complicated after HR. At the time of revision of a HR, the femoral neck can just be divided as in a 2 normal primary THR, making femoral revision no more difficult than a THR and much more straightforward than the femoral revision of a stemmed THR. The same amount of bone is removed on the acetabular side in both procedures making acetabular revision of a HR or a THR equivalent. With modern cup revision tools, bone ingrowth acetabular components can now be removed rapidly with minimal bone loss. Revising sockets without osteolysis is relatively straightforward.
- Dislocations are the most common cause for revision surgery after THR. They account for over 20% of all revisions. Dislocations occur in about 5% of all THR. About half of these cases become recurrent requiring revision surgery. They can even occur for the first time many years after the THR was done. Because of this problem, most patients after THR have to follow permanent lifelong restrictions to avoid suffering a dislocation. Dislocations occur primarily because most THR bearings are smaller than the original hip bearing that was replaced. This results in a biomechanically less stable joint that may dislocate. Fortunately, 95% of patients don’t have this problem. But we can dramatically reduce the risk of this complication by using a hip bearing that is the same size as the original hip. This is only possible with the thin‐helled acetabular components of large metal bearings. Either HR or THR with large (anatomic) sized metal bearings can achieve this stability. The risk of dislocation with these implants drops to less than ¼ % and typically only occurs early after surgery before the hip capsule has healed. After 6 months of healing no precautions are required.
- There never has been a case report of a breakage of a cobalt‐chrome metal bearing. I have one patient who has broken the peg of his femoral resurfacing component 5 years ago and is still functioning normally. I am not sure how this happened. But basically a HR is a pair of virtually indestructible cobalt chrome bearings. On the other hand, THR plastic liners are soft and breakable and ceramic is brittle and breakable. They are fairly durable to breakage, but long‐erm repetitive impact activities are not recommended with these implants. Recently, the size of these bearings has been increased from the previous standard 28mm to 32 and even 36mm to lower the risk of dislocation (explained above). The problem is that this requires that the plastic or ceramic liners must become correspondingly thinner, thus increasing the risk of breakage. These larger bearing implants have been in use for less than 5 years and few breakages have been reorted. Although newer plastic liners (cross‐linked polyethelene) are definitely more wear resistant, the tradeoff is that they are more brittle and may therefore be more prone to breakage at the location of the locking mechanism into the metal shell. Particularly when the liners are made thinner to accommodate larger head sizes. Impact activities are definitely not recommended. THR with metal on metal bearings also have indestructible cobalt chrome bearings, but the femoral head is sitting on top of a titanium stem with a metal neck set at approximately a 45 degrees angle. Stem breakage from fatigue failure was much more common with discontinued stainless steel stems of the past, but they have been reported with titanium stems. If implanted into young patients, after years of repetitive impact activities these stems may eventually break at the neck requiring splitting in half the top of the femur to extract a well‐fixed stem. Therefore metal on metal THR can tolerate higher impact, but extensive running should probably be avoided.
- Uncemented bone ingrowth femoral stems of THR are definitely more durable than cemented stems. But they do have a downside; in 3‐5% of modern designs the patient may experience thigh pain. Cemented THR stems do not cause thigh pain. Thigh pain can be caused by a loose femoral implant of any type. If the implant is not attached to bone, the implant rubs on the bone (micro motion) and irritates it. Failure of bone ingrowth into modern titanium porous coated stems is very rare; it occurs in less than 0.5% of cases. But some stems that are well fixed can still cause thigh pain. I believe this occurs because the titanium stem inside the femoral canal is much stiffer than the bone around it. When force is applied to the leg, the bone bends around the titanium stem. 3This differential motion irritates the femur in some patients and is the source of the “thigh pain”. If this problem occurs, there is no cure for it. This may be one of the main reasons why patients with THR have been found to be less frequently able to participate in high level athletics than those with HR. The inferior stability offered by smaller diameter bearings is the other possible reason.
- As the femoral head and neck is removed and a wedge shaped titanium stem is driven into the femoral canal a fracture of the femoral shaft can occur. Minor fractures that do not affect the outcome of the operation occur in 3% of cases. Displaced fractures that require surgery are seen in 0.7% cases postoperatively. These fractures are never seen after HR unless old hardware is removed from the proximal femur at the time of the HR surgery.
- Many patients who have severe arthritis of the hip are told that they need a hip replacement to solve this problem. They are also advised that after THR they should not perform physically demanding work, get into positions of extreme hip flexion or participate in many athletic activities. Many of these patients decide not to have a standard THR, but rather have a HR. This is one reason that study groups that have had a HR are generally younger and more physically active than study groups of patients with a THR. Therefore comparing the results of different studies of HR with THR is very difficult. Younger patients are on average much more demanding on their implants and are willing to accept fewer limitations without complaining. A young patient who wants to run is going to be unhappy if a femoral stem causes thigh pain, while an older person who just wants to golf may not ever be bothered by thigh pain with the same implant. Numerous studies have shown more normal gait and higher activity levels in patients with HR than THR. Recently a large multicenter comparative survey study found that in young patients that were highly athletic before their hip deteriorated were more likely to return to their previous activity level if they had a HR as opposed to a THR.
- Femoral neck fractures and collapse of the femoral head cannot occur after THR because this bone is removed. These complications occur in about 1.5% of HR cases within the first year after surgery. If they do occur, a revision surgery on the femoral side is required. Therefore 1.5% chance of failure can be said to be the cost of trying to preserve the proximal (top) part of the femur. It has long been known that women and older patients are at a higher risk for these complications. My research has now demonstrated that bone density (as measured by a DEXA scan) is the most predictive factor. Age and gender do not really matter; it is the DEXA scan number that really predicts the chance of fracture. Even better, recently completed studies show that these fractures can now almost always be prevented in patients with poor bone density by keeping them on crutches longer and treating them with fosamax. Therefore this complication now is much more rare! Even people with poor bone density can now safely have a resurfacing. But I would still avoid the operation in patients over 65 with poor bone quality.
- One of the most common problems with metal on plastic THR particularly in young patients has been an adverse reaction to wear debris. Younger patients are generally more active and wear out their bearing surfaces sooner. In patients under 60 the failure rate of older metal on plastic THR was 20‐0% at 8 years. Many of these failures were due to bone destruction caused by plastic wear debris. Plastic debris cannot be removed from the body naturally. It builds up locally around the hip. Cells called macrophages try to ingest it, but they rupture releasing chemical agents that destroy the bone. This has been called osteolysis due to plastic debris. Revising these cases can be very difficult because of the degree of bone loss encountered. Extensive bone grafting and specialized implants are often required. There is also typically a lot of soft tissue inflammation that must be cleaned out. Advanced bearings have been developed and tested in the laboratory. Metal on metal (cobalt chrome), ceramic on ceramic (alumina/zirconia), and ceramic on cross linked plastic (polyethelene) all show approximately 100x better wear tolerance than the original cobalt chrome against polyethelene bearings. I will call these modern bearings. It is expected that 4 the osteolysis problem will disappear with these modern bearings, which have now been available for 10‐12 years. However, adverse wear problems have recently been reported with modern bearings. Ceramic on ceramic bearings may develop extremely loud squeaking in 1‐% cases if an adverse wear problem develops. Bone or tissue destruction does not seem to occur, but revision is needed to get rid of the very bothersome noise. Imperfect positioning of the acetabular component is probably a major cause of this problem. Metal bearings may deposit excess cobalt and chromium in the tissues in rare cases causing inflammation and irritation of the local soft tissues. These have been called pseudotumors (false tumors). We have so far seen this problem in 0.1% of 3500 metal bearing cases over 12 years. This requires revision surgery. Although thorough debridement of the soft tissues is required in addition to revising the implants, we have been able to preserve all of the normal structures quite well; minimal bone destruction (osteolysis) is typically seen. This problem seems to be linked to placement of the acetabular component into a position that is too steep (high inclination angle) and sometimes also too tilted forward (anteversion). We have now developed intraoperative XR techniques that make acetabular component positioning more reproducible. Hopefully this will eliminate the adverse wear problems. Currently no comparative studies exist to show which modern bearing has the highest revision rate for adverse wear failure. It is likely that in all of these bearings the acetabular component position is the most critical factor.
- Numerous minimally invasive techniques have been developed for THR and even HR. I am not certain which operation should be called less invasive. An “approach” is what surgeons call the general method or direction that we use to enter the hip joint. Although all approaches used for THR can be employed for HR, most surgeons (90%) who perform HR do so through a fairly large (10‐12 inch) posterior approach. Many different approaches have been popularized for THR, but generally incision lengths are less (6‐8 inches). To move the femoral head out of the way and to gain access to the socket requires additional soft tissue releases that are not required for THR through the same approach. More internal cutting of soft tissue is required for a HR as compared to a THR when both are done through the posterior approach. But much less bone is removed in a HR than a THR. So which is less invasive? Blood loss and need of transfusion is another way to measure invasiveness of an operation. Many factors influence the need for a transfusion. Generally the national transfusion rate is about 30% for THR. There is little data on HR. In one randomized study the surgical blood loss was twice as high for HR when compared to THR and this was, in fact, listed as the reason to avoid HR in this Canadian study. Rapidity of recovery and return to normal function is another measure. Many studies have shown that generally minimally invasive techniques have sped up the recovery of patients when com pared to larger incision techniques for both THR and HR. Usually the final result is equal. However, in occasional studies, complications rates have been higher with minimally invasive surgery. The bottom line is that some surgeons are more skilled than others and are able to safely perform the same operation more precisely with a smaller incision and give their patient a small benefit of earlier recovery. I perform almost 90% my hip operations using a posterior minimally invasive technique. Most THR are done through a 3‐inch incision and most HR are done through a 4‐inch incision. Larger incisions are sometimes required if we have to reuse an old scar from a previous surgery, if the patient is obese around the hip or is extremely muscular around the hip, if old hardware needs to be removed, or if extreme bone deformity exists. HR is too difficult to perform in massive patients with BMI>40. They need to loose weight, or have a THR. Our blood transfusion rate is less than 5 0.1% for all primary hip surgery and the hospital stay is 1‐ days. I have not noticed any difference in speed of recovery between THR and HR. In a comparative study of incision size in HR done several years ago, we found that the final result was statistically better after 2 years in HR when minimally invasive techniques were used. The complication rate was the same for standard incision vs. minimally invasive surgery. In summary, both THR and HR can safely be performed using minimally invasive techniques by some skilled and experienced surgeons, decreasing pain, eliminating transfusions, minimizing the hospital stay, and speeding up recovery and return to normal function. Final function may also be improved. There is no difference in any of these factors including the rate of recovery bet ween a large metal bearing THR vs. a HR. It is advisable to review your surgeons published data on all of these factors.
- Early attempts at hip reconstruction in the 1950s involved both HR and THR. However, materials and technology at the time made HR less successful. Since that time the vast majority of operations have been THR. Clinical research of THR has been extensive. There is no question that much more long‐erm data is available for THR. However the results of traditional metal on plastic THR in young patients has been dismal. Fortunately, modern bearing technology has completely changed THR. Modern bearing THR and metal on metal HR have both been subject to extensive research in the last 12 years. Both show much improved success rates in higher demand younger patients. Both have about a 95% survivorship at 8‐10 years. (Only 5 of 100 patients have required revision surgery by the time they reach 8‐10 years) We call these midterm results. No long‐term data exists for either of these options. When some irresponsible companies advertise life spans of 20‐25 years for these implants, these claims are based on pure speculation, not scientific data. No good comparative studies exist. Few patients would likely allow themselves to be randomized into treatment groups of THR vs. HR. To further complicate matters, significant changes in implant design, manufacture and surgical technique has occurred in these last 12 years. Many of these innovations will improve both procedures; but some have already led to recalls. So which procedure has more long-term data? I think the answer has to be: Neither. Unfortunately, some surgeons who don’t perform HR or have not kept abreast of the scientific literature claim that there is less data on HR instead of discussing the true pros and cons with their patients. There is certainly much room for interpretation in the data, but all younger patients with severe hip arthritis at least need to be advised of the options. The only type of hip replacement that has published long‐erm data is an implant with a small metal on plastic bearing that has shown poor results in young patients. We have already dramatically exceeded these results at mid‐term follow‐up with all modern devices.
Is it better to resurface the hip or to perform a stemmed total hip?
There is much controversy among orthopedic joint replacement specialists about this topic. In the final analysis, the answer is not known because the few randomized studies comparing the two rival techniques are seriously flawed; a recalled implant system was utilized in both arms of these studies. When summarizing the scientific literature, it appears that both resurfacing and replacement using modern bearings have a similar overall 95% survivorship rate at 10 years. Longer‐term results are not available.
From a philosophical standpoint, hip resurfacing is the correct operation because it corrects the primary problem in hip arthritis without altering much else. The vast majority of severe hip arthritis cases are caused by the complete loss of the cartilage surface on both sides of the hip joint (femoral and acetabular). Replacement of these cartilage surfaces should be the goal.
Cartilage is a thin (3mm in the hip) layer of live material that covers the surfaces of all joints. It allows one bone to move smoothly against the other. Surface cartilage doe not have nerve receptors. If the cartilage surfaces are lost, bone rubs against bone. Bone has nerve endings that register this irritation and send a pain signal to the brain. This is the source of pain that is felt in a severely arthritic joint. A joint replacement is essentially a replacement of this cartilage layer by a pair of artificial implants. The goal is to remove enough bone to allow fixing an implant rigidly to each bone end. The implants then rub against one another. As long as the implants are fixed solidly to the bone, the arthritic joint pain is relieved.
Ideally, we would find a way to re‐row cartilage over these damaged surfaces. This is still a long way off in the future. In the meantime, hip resurfacing is the operation that alters the natural joint the least; it preserves the most native material and leaves the biomechanics of the hip the most normal. Therefore, in my opinion, it ought to be the way a hip joint is replaced.
Then why are most surgeons using standard stemmed total hip replacement?
Historically, the first hip replacements in the 1950s were hip resurfacings. However artificial materials available were not durable enough to allow thin replacement surfaces to work. The first type of hip replacement that can be said to have been truly successful was the hip replacement pioneered by John Charnley. He used a stainless steel stem and ball and a plastic (polyethelene) cup and cemented them into the bones with methylmethacrylate.
Much advancement in materials and techniques has now vastly improved upon his initial success. About 20 years ago, McMinn and Amstutz first recognized that materials were now good enough to allow resurfacing with thin metal bearings. This is when the modern era of metal on metal hip resurfacing began. I began performing hip resurfacing 12 years ago.
Today there is a large group of specialized joint replacement surgeons who are skilled at performing a standard hip replacement. Performing a hip resurfacing is very different technically. Preserving the head and neck of the femur makes it much more difficult to access the socket. In the standard hip replacement, after the head is removed, the socket is easily visualized. This is the primary reason why a surgeon who can quite skillfully perform a standard hip replacement may have difficulty with a hip resurfacing. If you can’t get adequate exposure of the joint with your approach, it is very difficult to place the implants properly. Most skilled hip surgeons could probably eventually learn how to do a hip resurfacing well. But there is a long learning curve. This means many complications may occur as the surgeon learns this new technique.
Few experienced hip resurfacing surgeons practice in academic teaching centers; as a consequence, new residents being trained are skilled at standard hip replacement, but not resurfacing. It is prob ably best that hip resurfacing is confined to relatively few high volume centers that can gain enough experience to identify the problems of this technique and develop solutions. This will limit the overall number of complications. For a patient interested in this procedure, it is best to bear the small additional cost and hassle to travel to an experienced surgeon with a good track record rather than take a chance on a local surgeon with little experience.
We look forward to serving you!