Joint Replacement Guide
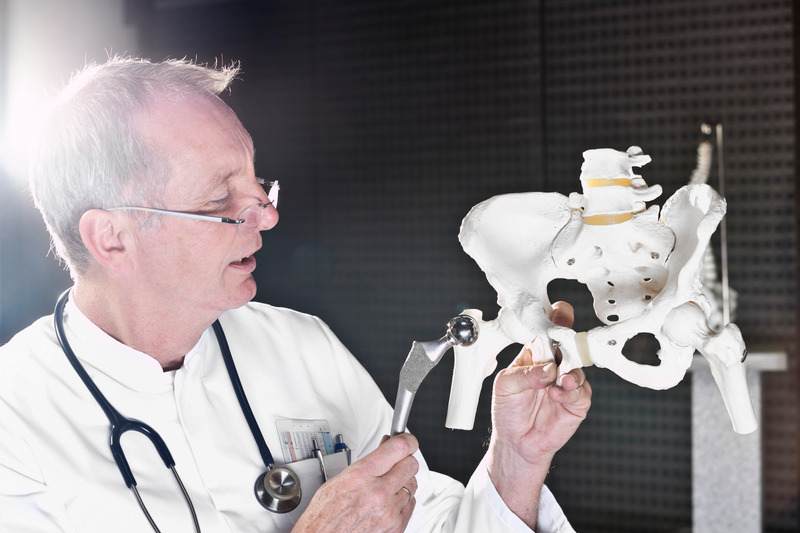
What is a hip or knee replacement?
It is a method to apply a new artificial lining to your joint when the natural cartilage has worn away. Typically, metal, ceramic, and plastic parts are used to accomplish this aim. Continue reading our joint replacement guide to learn more.
How long is the hospital stay for joint replacement?
Using minimal-invasive techniques and multimodal pain control, total joint replacement now only requires a 1 to 2-day hospital stay. We also offer many options for outpatient procedures. Thereafter, you may manage at home with a walker or crutches if you have someone to assist you with some daily activities. You will be able to walk and get in and out of bed or chair on your own. You will be taught stair climbing by the physical therapist and should be able to manage stairs on your own. You will be taught the appropriate stair-climbing techniques by a physical therapist which should allow you to manage stairs on your own. If you live alone and have no family or friends who can stay with you for the first week or two, a stay in a rehab center for this time would be advised. Partial knee replacement requires only a one-night stay in the hospital before going home.
View our Physicians to learn more of their expertise
When can I drive?
Total hips, total knees, partial knees, and hip surface replacement: whenever it is comfortable (1-2 weeks) to do so. You should drive an automatic and use your opposite leg for the brake, and you must be off all narcotic medications. Of course, you can ride in a car immediately upon discharge from the hospital.
Will I need a blood transfusion?
This depends primarily on your hemoglobin level before surgery. In young, healthy people if the level is above 13, 99% of the cases require no transfusion. Even in bilateral cases, transfusion is required less than 10 % of the time. No transfusion is generally required with a partial knee replacement. If your hemoglobin is below 13, we advise a series of Procrit (hematopoietic) injections usually given weekly for three weeks before surgery. These are quite expensive, but most insurance plans that have a drug benefit will pay for them. Another option is autologous blood donation. You deposit blood in the blood bank before surgery and use your blood after surgery. Most insurance plans will cover the cost of this service; however, it is less effective than preoperative Procrit injections. Revision (redo) surgery is more complicated than the initial joint replacement and often requires transfusion. Continue reading our joint replacement guide to learn more.
What is the risk of blood transfusion?
The risk of contracting AIDS is less than 1 in a million. The risk of hepatitis is approximately 1 in 2000. There is also a small risk of transfusion reaction. The risks of directed donor blood are the same as for the general blood pool.
How long is the recuperation period?
Recovery depends on the type of joint replacement that is done. It varies between individuals, but we can give you the following guidelines:
a. Hip Replacement (Resurfacing or Standard Types)
- 1 – 2 days in the hospital
- Use crutches for 1 – 2 weeks
- Use a cane for another 2 weeks
- Walking more than a mile without a cane and only a slight limp by 6 weeks
- Less pain than before surgery at 6 weeks
- Walking without a limp and climbing stairs foot-over-foot without a rail at 3 months
- Swelling of the leg for 3 – 6 months
- Maximum improvement at 6 – 12 months
b. Total Knee Replacement
- 2 – 3 days in the hospital
- Crutches/walker for 2 – 3 weeks
- Weight-bearing as tolerated
- Cane for another 2 – 3 weeks
- Physical therapy to gain range of motion for a total of 4 weeks
- Pain less than before surgery at 4 weeks
- Walking without a limp at 1 – 2 months
- Swelling and warmth around the knee for 3 – 6 months
- Maximum improvement at 6 – 12 months
c. Partial Knee Replacement
- Overnight stay in the hospital
- Physical therapy for 2 weeks at home
- Crutches/walker for 1 week
- Weight-bearing as tolerated
- Cane for another 1 – 2 weeks
- Pain less than before surgery at 2 weeks
- Walking without a limp at 2 – 3 weeks
- Maximum recovery at 3 – 6 months
Who is a candidate for joint replacement?
You are a candidate if you have severe pain in the hip or knee and if x-rays demonstrate bone-on-bone changes (cartilage worn completely off the end of both bones).
How do joint replacements work?
A normal joint is lined with a 4 mm layer of cartilage on either side of the joint. Cartilage has no nerves. It provides a protective layer for the bone ends that move against each other in any normal joint. When the cartilage starts breaking down, the joint becomes inflamed and starts hurting. At this stage, the symptoms are mild and medications usually help relieve the pain. However, when the cartilage completely wears through, the bone ends begin directly rubbing against each other. Nerve endings in the bone are stimulated, resulting in significant pain. At this stage, the diagnosis is severe arthritis. Pain medicines usually do not give adequate relief and most people are forced to substantially curtail their activities. The principle of any joint replacement is to provide a new artificial joint-bearing surface that is fixed to the bone on either side of the joint. Motion of the joint now no longer causes the bone ends to rub against each other. As long as the implants remain well fixed to the bone on either side of the joint, motion no longer stimulates the nerve endings in the bone, and motion is painless. Activities can be resumed without pain. Continue reading our joint replacement guide to learn more.
Can I manage at home after hospital discharge?
Most people can do well at home as long as a friend or relative can provide some assistance. If you have a new replacement, a physical therapist will come to your home for one month.
Will I have post-op pain?
Very little with modern, multimodal pain management techniques. In the past, both hip and knee replacements have been very painful procedures. As a rule, most people now are quite comfortable after surgery. The only people who do still have pain that is difficult to control are persons addicted to prescription narcotics before surgery. We use several different methods in combination to minimize post-operative pain, and minimally invasive surgical techniques are used whenever possible.
Spinal Anesthesia
The anesthesiologist will give you sedation, numb your skin and place numbing medication along with a long-acting narcotic into your spinal canal. This method cuts down on blood loss and blood clots, and it provides hours of pain relief.
Local Anesthetic Infiltration
Before closing your wound, we inject a local agent into your tissues to help provide post-operative pain relief. Platelet concentrate is used to decrease pain, speed up healing, and minimize blood loss during surgery.
Ice Machine
Continuous circulation of ice water through a pad placed next to the surgical site aids in pain control and decreases swelling.
B Patient-Controlled Analgesia (PCA Pump)
This can be used for breakthrough pain control. It allows you to push a button when you feel pain and cause Morphine or Demerol to be directly infused into your vein for immediate pain control (no need to wait for a nurse to bring pain medicine).
Oral Narcotics
We use Oxycontin as a preemptive and continuous long-acting narcotic while you are in the hospital to prevent pain. Typically, Vicodin is used for additional pain control and is continued after the other methods (above) are no longer needed.
Anti-Inflammatory Drugs
Celebrex or Mobic is given in the preoperative holding area and used throughout your hospital stay and for one-month post-op. These decrease the need for narcotics and improve pain control (The fewer narcotics a patient requires, the better, because the side effects include confusion, nausea, itching, and constipation.)
How long will I be out of work?
If you do a sedentary job, you may return in 1 to 2 weeks. If you do a good bit of walking, you should wait for 6 to 8 weeks to return. Heavy labor-type work should be avoided until 6 months post-op.
What equipment is needed post-op?
The Physical and Occupational Therapy Department at the hospital will make arrangements for you to purchase a walker or crutches, raised toilet seat, a reacher, and other equipment as needed. If you already have this equipment, please bring it with you to the hospital.
What clothes should I bring to the hospital?
To enhance your postoperative therapy, a knee-length robe or gown is recommended. Do not bring floor-length robes as they make walking difficult.) Ladies may want to bring a camisole or lightweight cotton shirt to wear under the hospital gown for added warmth. Leave all jewelry at home! A package containing personal care items is provided. Loose-fitting pajamas, shorts, or sweats are useful to wear on the way home. Bring comfortable, slip-on shoes with non-skid soles. Of course, good reading material may help pass the time more quickly. Continue reading our joint replacement guide to learn more.
Can I fly home on the day of discharge?
Most of our out-of-state patients are discharged from the hospital on the second post-op day, stay overnight in a hotel, and fly home the next day. We do have patients that wish to stay an additional night in a local hotel and fly home the next day. Your spouse may stay in your hospital room; the staff will supply a recliner or cot. There is an airport in Columbia, S.C. that is 15 minutes from the hospital. Also available is an airport in Charlotte, N.C. It is about an hour and a half away and is an international airport that offers more direct flights than Columbia. We have patients leave the hospital, ride to Charlotte, stay overnight there, then fly home.
Will you provide me with detailed written discharge instructions?
Yes, we provide you with detailed written discharge instructions as well as your exercises. The nurses and physical therapists at the hospital will review all of these in detail with you. You should understand all of the instructions before discharge. The forms will simply serve as a reminder.
Will I be able to climb stairs?
Yes, you will be instructed in stair climbing by the physical therapist during your hospital stay. If your bedroom is upstairs, you will be able to manage this once you get home.
Will I need physical therapy once I get home?
For patients undergoing hip surgery, you will be given a detailed physical therapy program during your hospital stay. Once you are discharged to your home, you will continue this program on your own three times a day. The best therapy is to institute a formal walking program and increase your distance daily. At six weeks post-op, we will progress you to the Phase 2 hip exercises (form #7 on the website). For patients undergoing knee surgery, physical therapy will be arranged for you by our medical social worker. You will have physical therapy every day for the first week then three times a week for the next three weeks. For patients undergoing a unicompartmental replacement, you will follow the same regimen but it will only last two weeks, then you will continue therapy on your own. Continue reading our joint replacement guide to learn more.
How long will my joint replacement last?
This depends primarily on a person’s activity level. A tire on a car wears out in a shorter period when the car is driven many miles per day. Similarly, younger patients typically wear out an artificial joint faster because of a higher level of physical activity. In general, a standard metal/plastic joint replacement in a person older than 65 usually lasts approximately 10-15 years. In a more active 40-50-year-old patient, this type of replacement may only last 5-7 years. Fortunately, we now have metal/metal bearings (hips) that can tolerate 10-1000 times as much wear as the older metal/plastic bearings and therefore last much longer.
Thank you for reading our joint replacement guide!